The placebo effect, a phenomenon where patients experience real improvements in their symptoms after receiving a treatment that has no therapeutic value, has intrigued scientists and clinicians for decades. This report provides an in-depth look at how placebo effects work in medicine, drawing exclusively from available texts[1][2][3][4][5][6].
Mechanisms of the Placebo Effect
Psychosocial and Expectation-Based Mechanisms
Placebo effects arise primarily from the psychosocial context and the expectations of the patient. Positive outcomes are often linked to the patient's anticipation of relief, which in turn activates various neurobiological pathways[1]. When a patient expects pain relief, their cognitive and emotional circuits are engaged, resulting in the release of endogenous opioids and other substances that modulate the sensation of pain[1]. This expectation-driven activation involves the dopaminergic, opioidergic, vasopressinergic, and endocannabinoidergic systems, which are crucial for the placebo-induced benefits observed in pain management and other symptoms[1].
Behavioral Conditioning
Conditioning is another significant mechanism behind placebo effects. Classical conditioning involves pairing a neutral stimulus with an active treatment, leading to the neutral stimulus eventually eliciting the same response as the active treatment. Studies have shown that placebo effects can be conditioned to mimic the action of medications, such as immunosuppressive drugs, by using a novel taste as a conditioned stimulus[1][3].
Perception and Mindsets
Patients’ mindsets, which are shaped by various factors including societal norms and prior experiences, play a pivotal role in the effectiveness of treatments. For instance, mindsets about the capacity to change and the efficacy of treatments can significantly influence health outcomes. In a study where room attendants were informed that their work was equivalent to exercise, those informed showed significant health improvements despite no actual changes in their physical activities, indicating the profound impact of mindsets on health behaviors and outcomes[3].
Neurobiological Underpinnings
Neural Circuitry
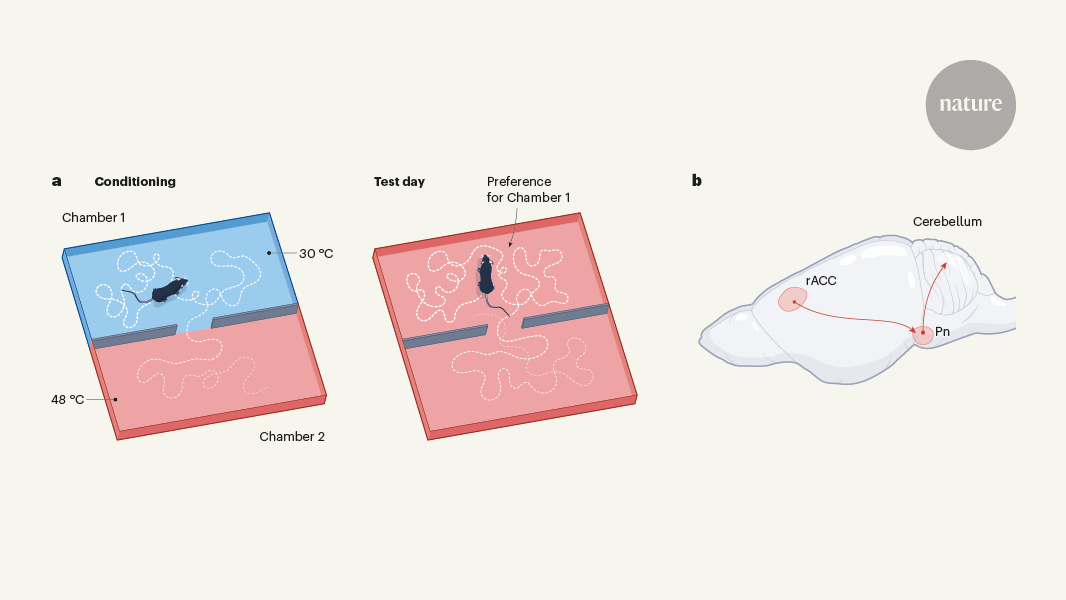
Recent studies have identified specific brain regions involved in placebo effects. For example, research on placebo pain relief using mice has pinpointed neurons in the limbic system that mediate the expectation of pain relief and send signals to the brainstem and cerebellum, regions typically associated with movement coordination[4]. This unexpected finding highlights the complexity and breadth of neural mechanisms involved in placebo effects.
Reward and Pain Modulation Systems
The placebo effect also engages the brain’s reward and pain modulation systems. The descending pain modulatory system (DPMS) and the reward system are key players. The DPMS includes regions like the cingulate cortex and prefrontal cortex, projecting to the periaqueductal gray and rostral ventromedial medulla, which are involved in pain inhibition[5]. The reward system, involving the nucleus accumbens and cerebro-dopaminergic pathways, plays a crucial role in how expectations influence pain perception and overall treatment outcomes[5].
Placebo Effects in Clinical Practice
Application and Challenges
Clinicians have long leveraged placebo effects, sometimes using treatments like “bread pills” or colored water to produce subjective improvements in patients[3]. The effect of placebos is not limited to deceptive administration. Open-label placebos, where patients are aware they are receiving a placebo, still produce significant health benefits[1][6].
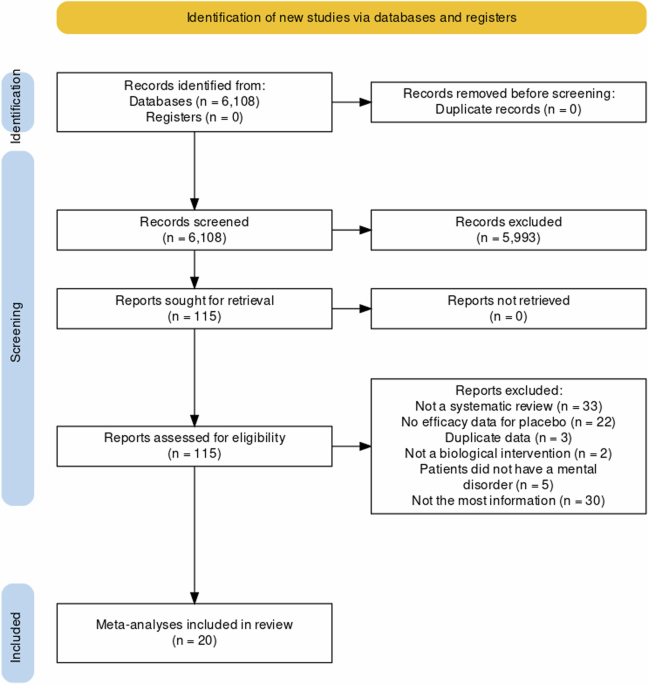
In clinical trials, placebo effects pose a challenge as they can confound the assessment of a drug’s efficacy. Measures like placebo run-in periods, where patients initially receive a placebo without their knowledge, have been used to minimize these confounding effects, although their impact on trial outcomes varies[2].
Ethical Considerations
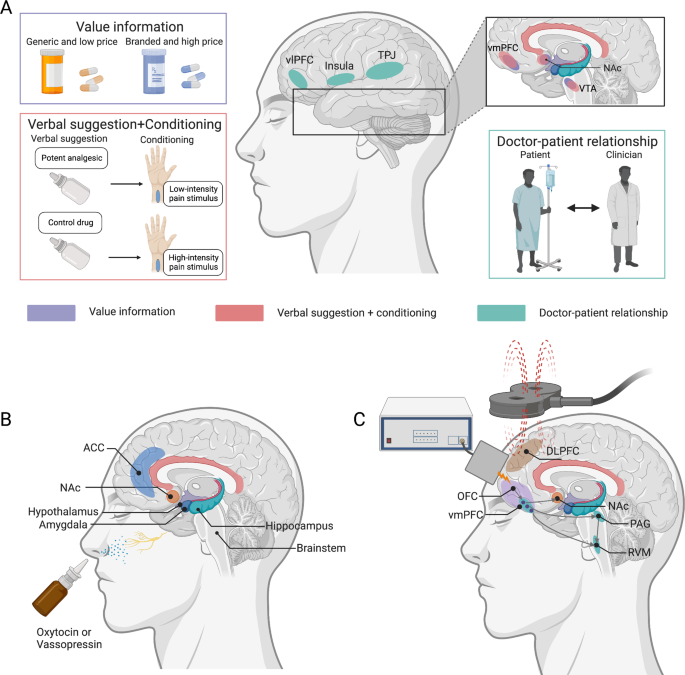
The ethical use of placebos in clinical settings remains contentious. While placebo effects can significantly improve patient outcomes, using deceptive methods to administer placebos raises ethical concerns. Thus, open-label placebos and dose-extending placebos, which combine real medications with periods of placebo administration, are considered more ethically sound alternatives[1][5].
Future Directions
Personalized Medicine and Placebo Responsiveness
Future research aims to better understand the individual variability in placebo responsiveness. Factors such as genetic predispositions, psychological traits, and prior treatment experiences influence how patients respond to placebo treatments[1][3][5]. Advancements in neuroimaging and computational modeling are expected to further elucidate these individual differences, paving the way for more personalized medical interventions that maximize therapeutic outcomes by enhancing placebo effects.
Integrating New Technologies
Non-invasive brain stimulation techniques like transcranial magnetic stimulation (TMS) and transcranial direct current stimulation (tDCS) are being explored to modulate placebo responses. By targeting specific brain regions involved in expectation and pain processing, these techniques have the potential to enhance placebo analgesia and other beneficial placebo responses in clinical settings[5].
Conclusion
The placebo effect, once seen as a mere nuisance in clinical trials, is now recognized as a potent therapeutic agent. Understanding its mechanisms—ranging from psychosocial factors and conditioning to complex neurobiological pathways—offers valuable insights into enhancing patient outcomes. As research continues to unravel the intricacies of placebo effects, integrating these findings into routine clinical practice presents both opportunities and ethical challenges that must be carefully navigated.
By incorporating psychosocial, pharmacological, and neuromodulation strategies, healthcare providers can potentially harness the power of placebos to improve therapeutic outcomes while maintaining ethical standards. The future of placebo research promises to refine these applications further, contributing to the advancement of personalized and effective medical care.
Get more accurate answers with Super Pandi, upload files, personalized discovery feed, save searches and contribute to the PandiPedia.
Let's look at alternatives:
- Modify the query.
- Start a new thread.
- Remove sources (if manually added).